By Vivian Ihechu
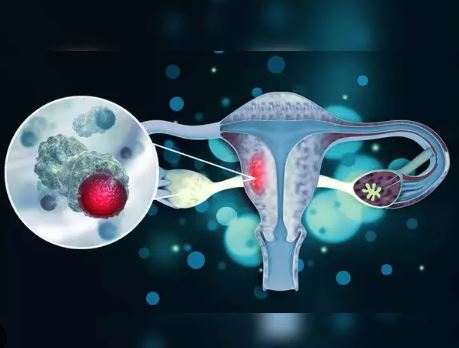
Cervical cancer is the second most common cancer affecting women in Nigeria and the fourth most common cancer among women globally, according to World Health Organisation (WHO).
Current estimates for Nigeria in 2023 by the Human Papillomavirus (HPV) Centre indicate that every year 12,075 women are diagnosed with cervical cancer and 7,968 die from the disease in the country.
About 3.5 per cent of women in the general population are estimated to harbour cervical HPV-16/18 infection at a given time, and 66.9 per cent of invasive cervical cancers are attributed to HPVs 16 or 18.
However, with proven interventions to prevent and manage the disease, experts say that no woman is expected to lose her life to cervical cancer.
Prof. Isaac Adewole, a former Minister of Health, Nigeria and Co-Founder, African Cancer Coalition, told NAN in Lagos that cervical cancer had become a public health issue.
Nevertheless, Adewole, a professor at the University of Ibadan and Northwestern University, said the disease which was caused almost entirely by a virus, could be tackled.
He said cervical cancer was preventable and treatable, if presented and diagnosed early.
He said part of the strategies to eliminate cervical cancer included, vaccination of about 90 per cent of girls between ages nine and 14 with HPV vaccine to prevent them from having the cancer.
According to him, it takes about an average of 20 to 30 years for cervical cancer to develop, and the HPV vaccination offers a window of opportunity to kick against the cancer.
He said screening of no fewer than 70 per cent of women using a high-performance test by the age of 35, and again by the age of 45, was also a strategy to save women from cervical cancer.
“When we screen women who are asymptomatic, we have no complaints at all.
“When we screen them, we’ll be able to determine and diagnose stages that occur before development of cancer. We call these stages pre-malignant stages.
“We are able to detect them and when we offer appropriate treatment they will be cured,” said Adewole.
A third way of addressing the cervical cancer menace, according to Adewole, is prompt and appropriate treatment when detected early.
“Even those who develop cervical cancer, when we pick them in the early stages, we can almost uniformly cure them.
“Treatment of women with early presentation as well as invasive cancer management helps.
“When you look at the three factors of prevention, screening, which is secondary prevention; and treatments of early stages, we have a disease on our hands that applying public health principles, we can control,” explained the professor.
Adewole advocated allocation of resources for cancer prevention, detection, treatment and management.
“Cervical cancer disease is common in areas that are not developed or areas where they have not allocated appropriate resources and attention to this disease.
“It is a disease of under development.
“And where you have infrastructure well developed, where you have appropriate policies that are well-resourced, where you have leadership showing interest in this disease, we collectively can eliminate cervical cancer.
“And this has been amply demonstrated through projections scientifically showing that if you do this, then cervical cancer can become something of history,” said Adewole.
According to him, the challenge in Nigeria, just like in Africa and many developing countries, is that a lot of people are largely unaware of the situation with cervical cancer.
Therefore, he said when cases were presented to the hospitals, they were largely in advanced stage, for quite a number of reasons.
The former health minister also noted that the non-availability and affordability of vaccine hindered efforts in the drive to eliminate cervical cancer in Nigeria.
“It is very expensive if you go to the shelf to buy it and then, globally, the developed countries have ‘cornered’ the vaccine for their people because they recognise the value of the vaccine.
“So, we are left at the mercy of Gavi, the Vaccine Alliance (GAVI) and multilateral donors to fund us.
“The prices are coming down gradually but it is still out of reach for most groups.
“But, there is a window or door of opportunity for many as countries that were previously giving two or three shots can now give one and that will free some of the supplies,” continued Adewole.
He said by adopting, introducing and implementing the Global Elimination Agenda for Cervical Cancer Control https://www.cervicalcancerdeclaration.org/, eliminating cervical cancer as a public health issue would be realised.
“Hence, we call for urgent action to make cervical cancer elimination a global priority, with high-level commitment and resources to make it a reality.
“No woman should lose her life to cervical cancer when we have the tools to prevent, and, especially when diagnosed early, to treat it,” he said.
HPV is mainly transmitted through sexual contact and most people are infected with HPV shortly after the onset of sexual activity.
Twelve leading health experts from around the world have initiated a call to action in the fight against cervical cancer through The Global Declaration to Eliminate Cervical Cancer.
The Declaration was formally launched at the World Health Assembly in Geneva on May 22, with signatures from more than 1,200 global health leaders and advocates representing no fewer than 100 countries.
Top among them included former Prime Minister of New Zealand, Jacinda Ardern, CEO of Amref Health Africa, Githinji Gitahi; President of the International Federation of Obstetrics and Gynecology (FIGO), Jeanne Conry, and President-elect of the International Pediatric Association, Naveen Thacker.
Adewole and Prof. Margaret Stanley of Cambridge University, UK and Past President of the International Papillomavirus Society (IPVS), are among the experts championing the declaration.
Stanley told NAN that it was worrisome that 90 per cent of women with cervical cancer lived in low and middle income countries.
According to her, in high income countries like U.S., UK, Europe, there are highly organised medical services which women can access easily.
She added that same services should be replicated in low income countries like Nigeria.
Stanley also agreed that no woman should die from cervical cancer as eliminating the disease was achievable with urgent action in three areas – vaccination, screening and treatment.
“Vaccinating girls aged nine to 14 against HPV is the primary way to prevent cervical cancer.
“HPV vaccines are safe, effective, and can prevent up to 90 per cent of cervical cancer cases.
“Cervical cancer can also be prevented through screening and treatment of pre-cancerous lesions,” said Stanley.
She also recommended the ‘new’ one-dose HPV vaccination regime as part of routine programmes for girls.
The British virologist and epithelial biologist also called for provision of X rays for screening for cervical cancer, while advocating increased access to adequate health facilities and trained health personnel.
According to experts, tools are available to eliminate cervical cancer and everything must be engaged collectively to eliminate the disease and save women from losing their lives to cervical cancer.
NAN